In October 2024 the Network initiated a regional project for the National Cancer Improvement Collaborative (Experience of Care), with its providers the Christie, the Clatterbridge Cancer Centre and Alder Hey.
Experience of care: Improvement collaboratives
The Cancer Experience of Care Improvement Collaborative brings together groups of cancer healthcare professionals and people with lived experience from different organisations to work in a structured way to improve services. Its aim is for each project team to use insight and feedback (e g Cancer Patient Experience Survey results) to improve the experience of care for cancer patients, their families, and unpaid carers. Project teams can make improvements based on what matters to people who use cancer services that align with local, regional, and national priorities.
NHS England » Experience of care: Improvement collaboratives
Cohort 6 had a focus on administration of care and asked for expressions of interest around improvements in this area.
The NWTYA team met monthly to undertake a series of quality improvement methods to understand any gaps in administration of care. Each centre provided their late effects pathways, tools and resources and agreed a SMART AIM – “To ensure all TYA Patients in the North West Network have access to an end of treatment summary and late effects information”.
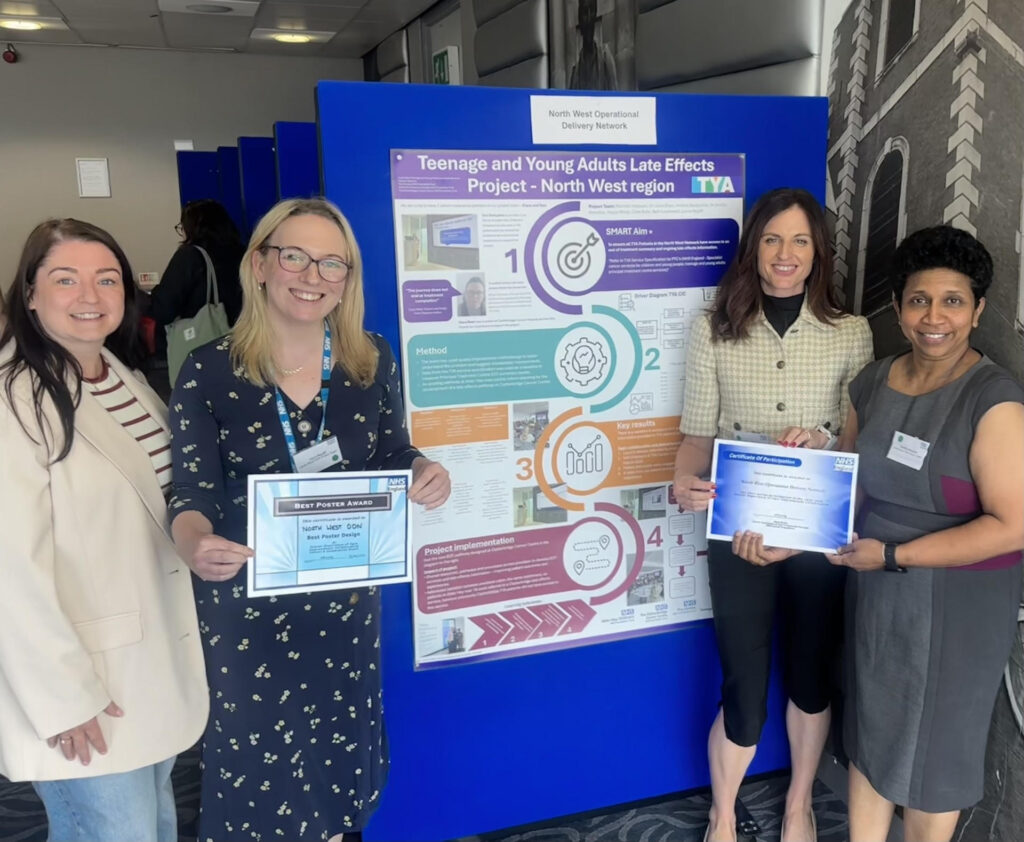

The the project team Toni Derbyshire, After Cure Nurse Alder Hey, Laura Bayliff the TYA Network, Rachael Hastwell, TYA Programme Manager, Dr Sindhu Retnabai, Speciality Doctor in TYA the Christie.
Rachael Hastwell with Neil Churchill (Director for People and Communities at NHS England
Engagement: People with Lived Experience (LEP)
The Project Team have two lived experience partners; one was a patient at the Clatterbridge Cancer Centre and the other is an After Cure Nurse who was also a TYA patient and shared both their professional and personal experience.
A quote was provided by the LEP
“The journey does not end at treatment completion” – Lived Experience Partner
“People with lived experience actually makes you change your thinking and enables you to pause and reframe to avoid jumping in with the solution” – Project Lead
Engagement: Staff and Patients
The Project Team have engaged with a wide range of staff including medical, nursing and service staff from across the three providers as well as wider network representatives.
“Having those members of staff on the Project Team helps to progress it” – Project Lead
Impact
The Project Team learned about variation within their own region and by collaboration have understood the gaps in the pathway. They are sharing resources, pathways and processes across providers to support and develop the service. The Project Team have used methodology to understand the issues and develop their key objectives. They continue to work with patient partners to develop improvements.
“The project reinforces why it’s so important why everyone get the same service” – After Cure Nurse & LEP
“Patients don’t understand and it’s about advocating for them to make sure it’s as good as it can be for them” – Project Lead
Next steps
The Project Team will meet in July to review progress against new pathway implementation but also consider resources and shared learning from the project.
Additionaly there will be a 6-month review held in November with the National Cancer Improvement Collaborative team to discuss further actions and developments.




